Case of the Week #629
(1) Ukraine, Kyiv; (2) Centro Médico Recoletas, Valladolid, Spain; (3) Femicare, Center of prenatal ultrasonographic diagnostics, Martin, Slovakia
A pregnant woman with unremarkable past medical history presented at 20–21 weeks gestation. This is her second pregnancy. She has had one previous delivery and a healthy child.





View the Answer Hide the Answer
Answer
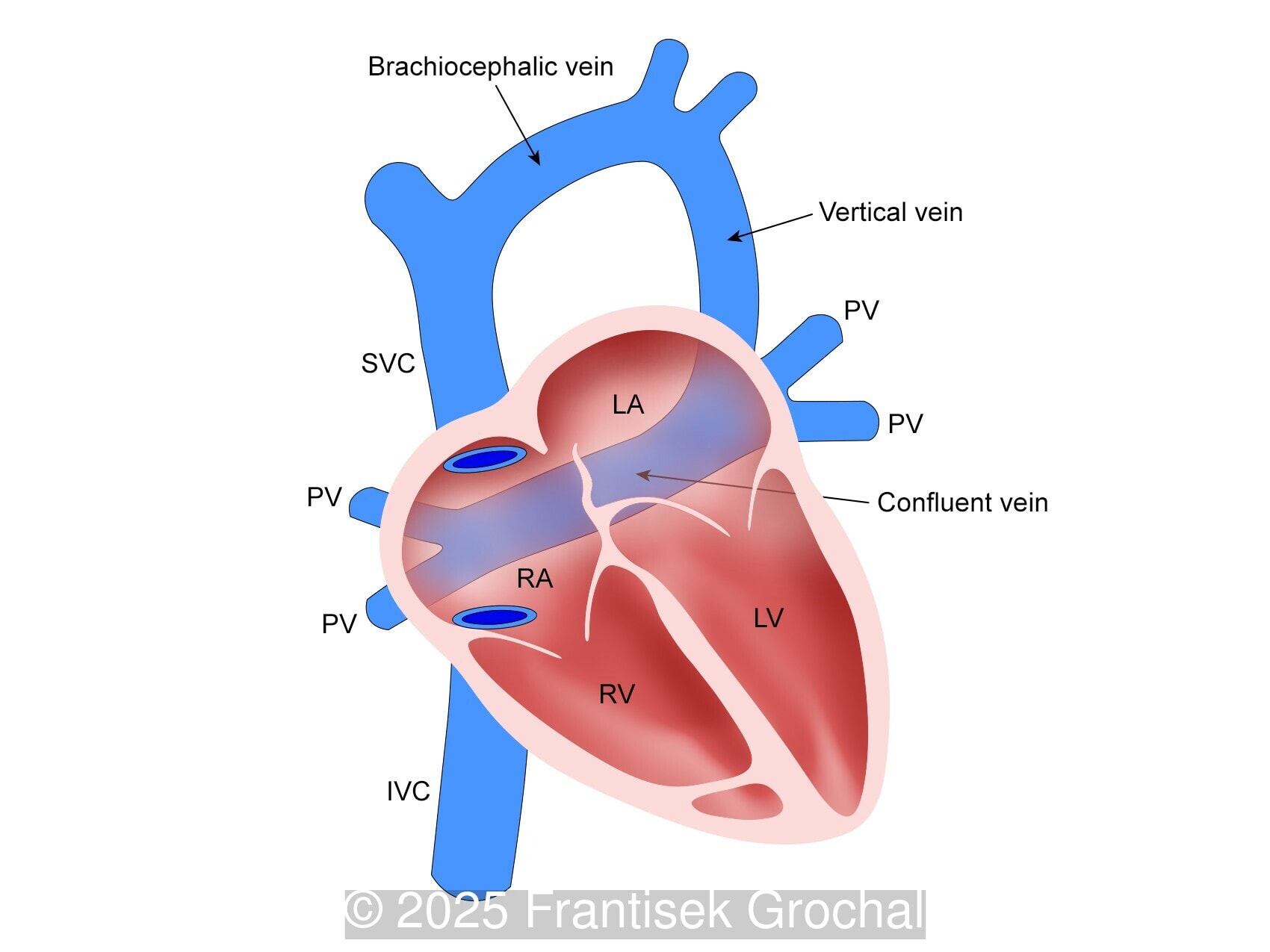
We present a case of total anomalous pulmonary venous return (TAPVR), supracardiac type.
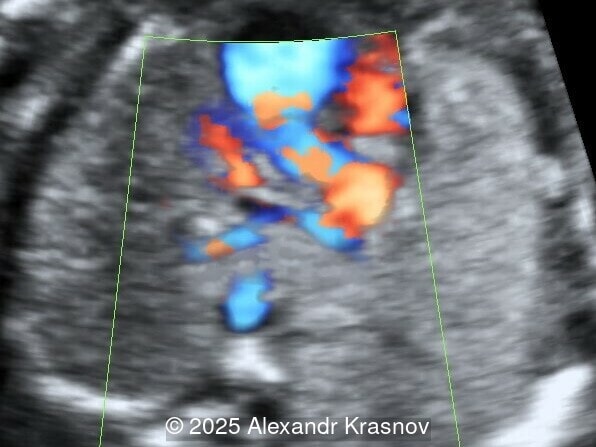
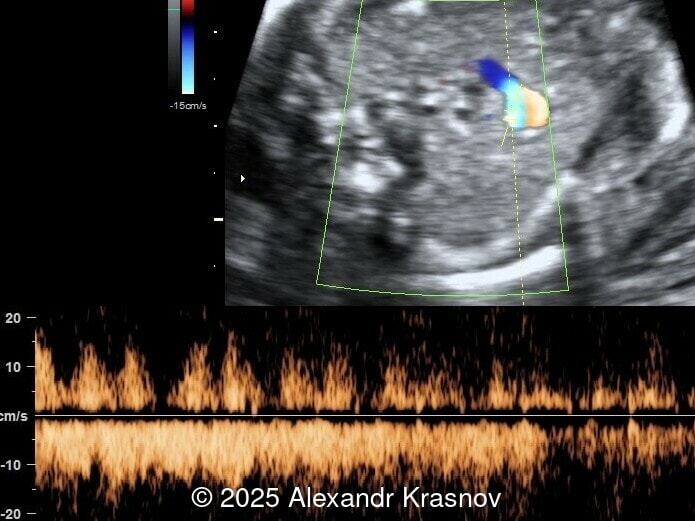
Our ultrasound showed biometry data corresponding to 21 weeks of gestation. During echocardiography, an abnormal drainage of the pulmonary veins was detected in which the pulmonary veins drain into a venous collector linked to the superior vena cava. The four-chamber view and the three-vessel view were altered and raised suspicion of a pathology. The grayscale and color Doppler images of the four-chamber view indicate a smooth posterior wall of the left atrium, increased distance between the left atrium and the descending aorta and the absence of pulmonary veins entering the left atrium (Image 1, 2; Video 1, 2). In the three-vessel view, the diameter of the superior vena cava appears larger than that of the aorta (Image 3, Video 3). In the images of the venae cava, a significant difference is seen between the diameters of the inferior and superior vena cava with significant enlargement of the superior vena cava (Image 4, Video 4). Additionally, there is a pulmonary venous confluent chamber (“twig sign”) behind the left atrium (Image and Video 5). A vertical ascending vein connects the confluent chamber with the superior vena cava where it drains blood from the pulmonary veins (Images 6, 7; Video 6).
The patient was referred to the State Institution "Center of Cardiology and Cardiac Surgery" of the Ministry of Health of Ukraine, where the diagnosis was confirmed. At the family's request, the pregnancy was terminated.
Discussion
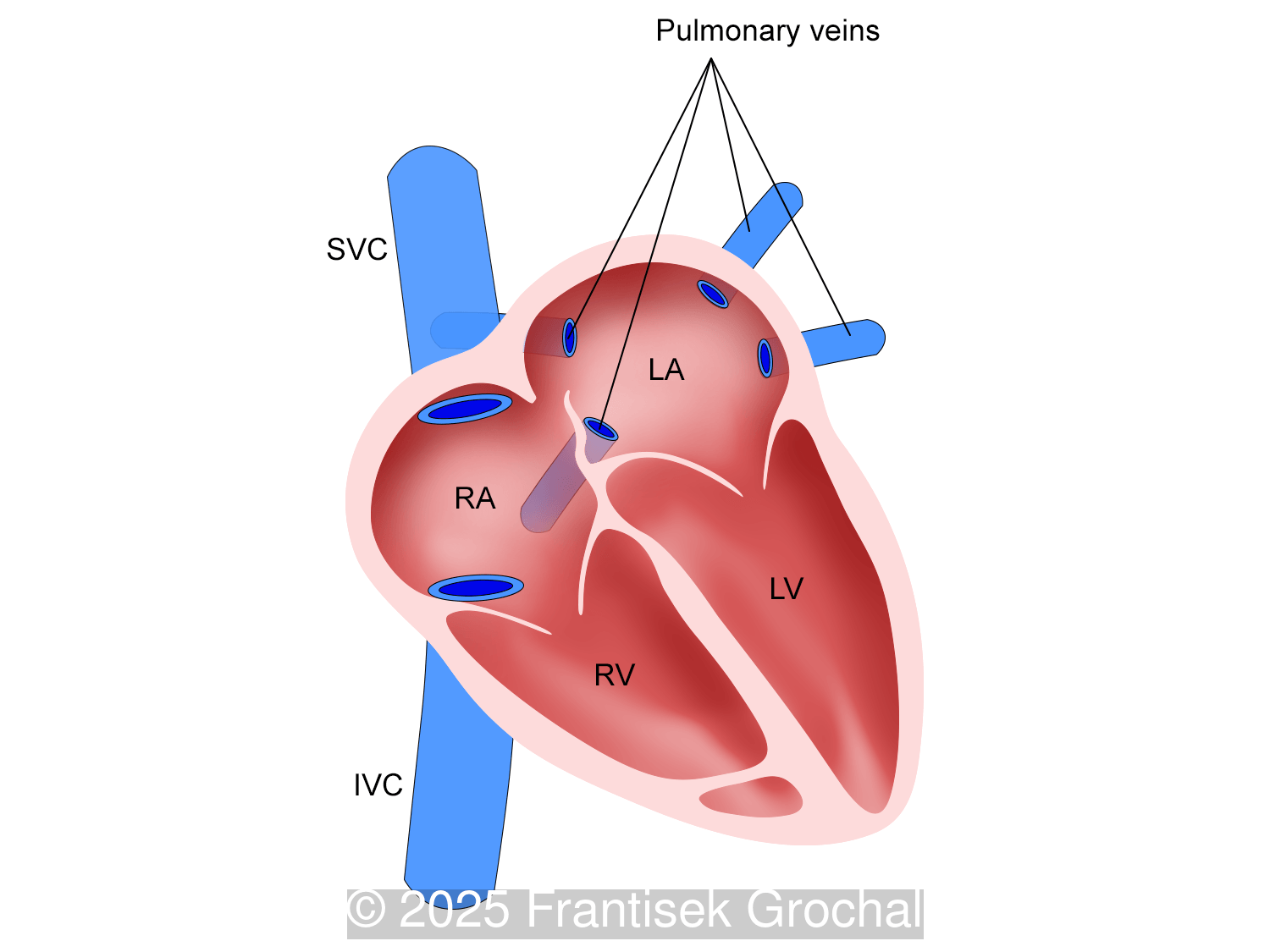
Anomalous pulmonary venous return, connection, or drainage is a heart defect in which one or more pulmonary veins which normally empty into the left atrium do not do so. Anomalous pulmonary venous return may be partial, where only one or several veins drain directly or indirectly into the right atrium, or total (TAPVR), in which all veins have abnormal drainage [1]. Typically in TAPVR, all four pulmonary veins from both lungs join a single large vessel - a collector - that connects to the systemic venous system.
In the Baltimore-Washington Infant Study, a population-based exploratory case-control study of cardiovascular malformations, the prevalence of TAPVR is 1 in 14,705 live births, which represents 1.5% of all congenital heart diseases [2]. Although it may be an isolated finding, it is usually found in the context of right isomerism and, more rarely, associated with syndromes such as Holt-Oram and cat eye or chromosomal abnormalities [1].
Darling et al developed a classification system for TAPVR in 1957, which describes the pattern of pulmonary venous drainage into the systemic venous circulation [3]:
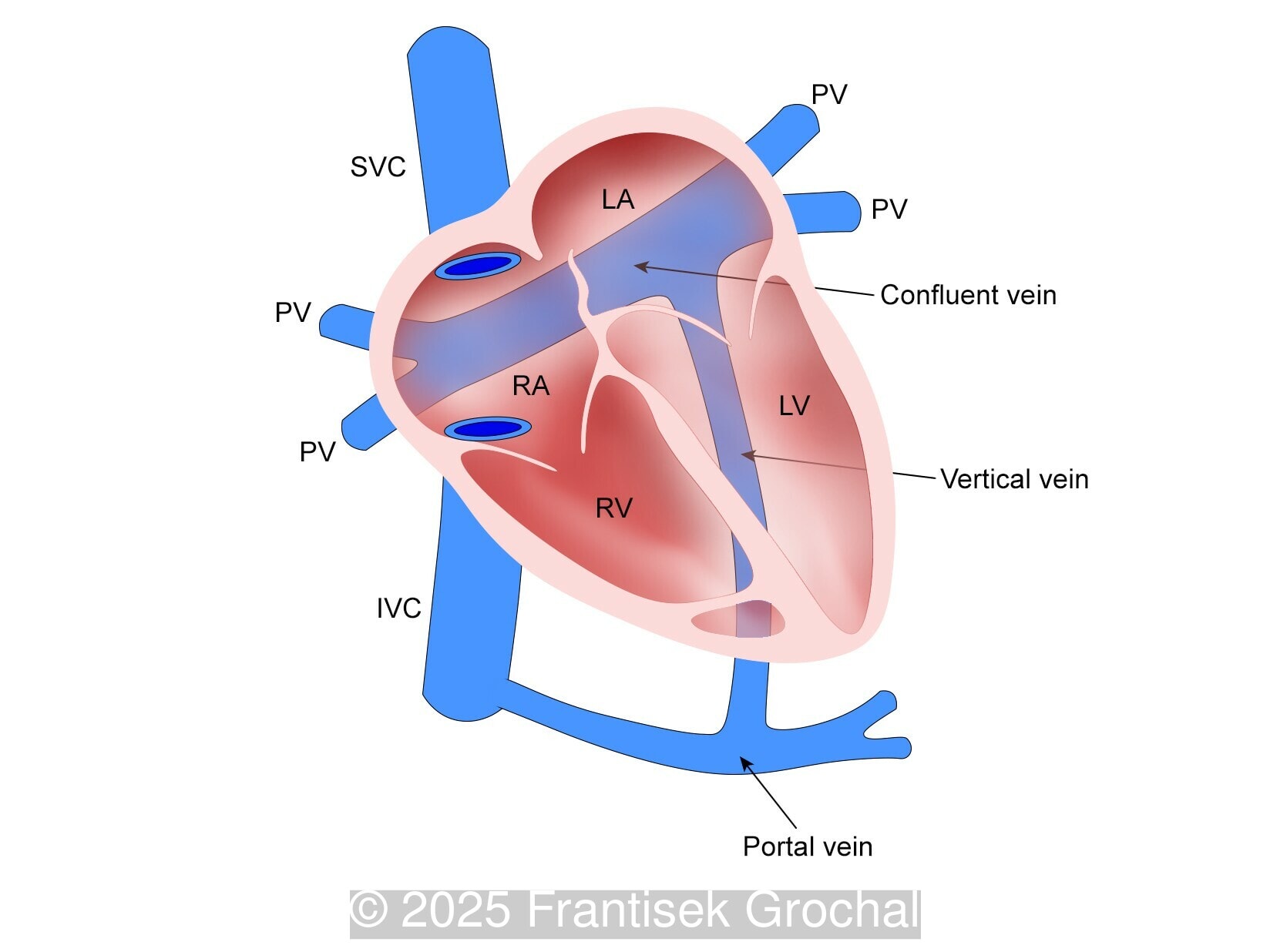
- Supracardiac (50%) – the blood collected in the venous collector flows through a vertical vein to the innominate vein, superior cava and right atrium
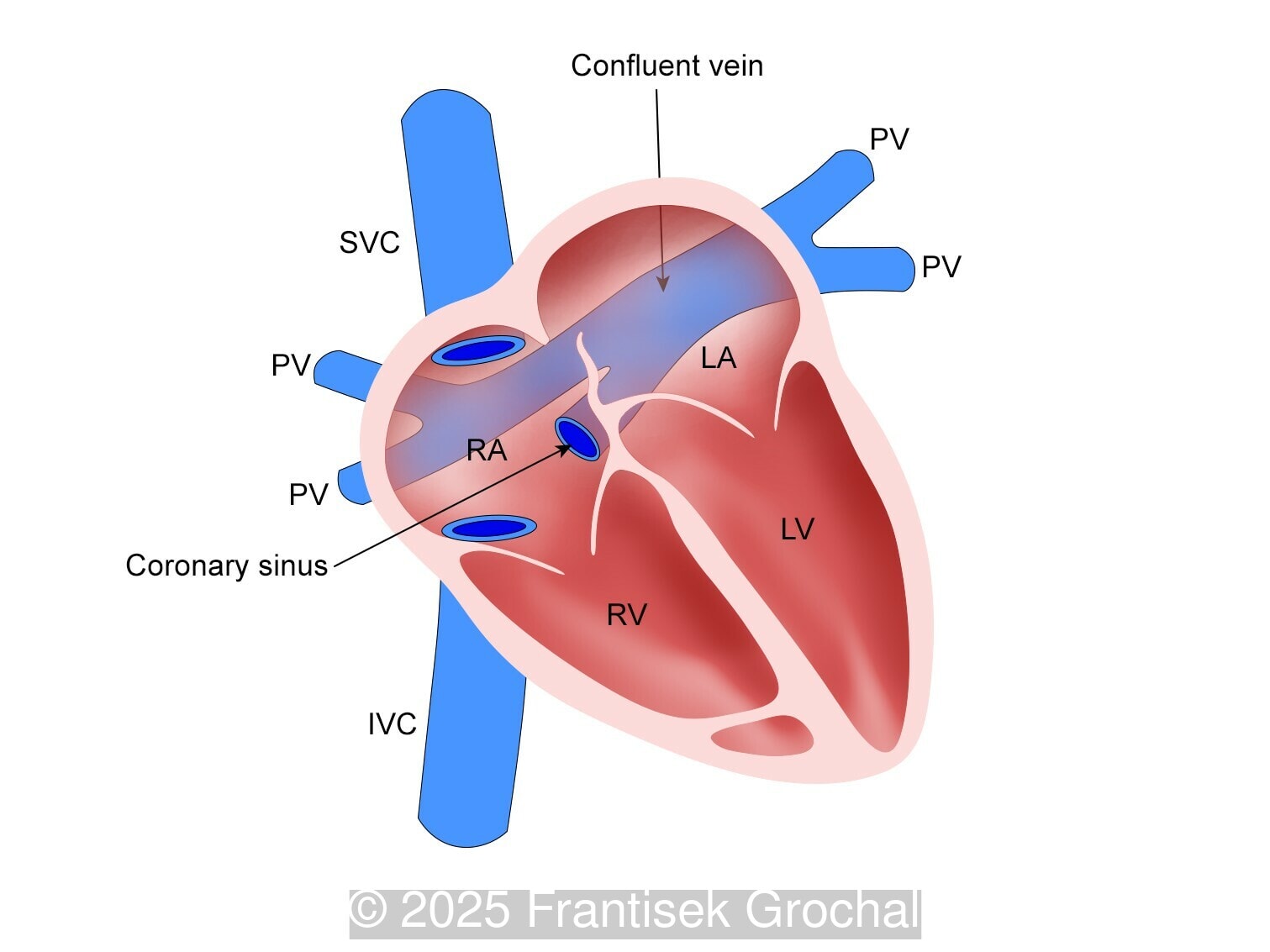
- Cardiac (20%) – blood enters through an enlarged coronary sinus (the most common) or directly into the right atrium
- Infracardiac or infradiaphragmatic (20%) – the collector continues via a vertical vein that crosses the diaphragm, usually draining into the portal vein or, more rarely, into the ductus venosus or the inferior vena cava.
- Mixed (10%)
Diagnosis of anomalous venous return in fetal life is a challenge, with prenatal detection rates that vary between 0% and 50% [4]. Clear and unequivocal visualization in B-mode or color Doppler at a low velocity range of any pulmonary vein entering left atrium excludes the diagnosis of TAPVR. When the connection between the pulmonary veins and the left atrium is not clear, the diagnosis should be confirmed based on several sonographic markers, commonly classified as direct or indirect [5].
Direct markers are based on anatomical features in TAPVR, and their presence usually confirms the diagnosis. Some appear in all types of TAPVR, and others are specific to particular types. A lack of connection between the pulmonary veins and the left atrium or the presence of a confluent chamber can be found in all types of TAPVR. Whereas the presence of an ascending or descending vertical vein is found in supracardiac or infracardiac types. Normal entry of a left and right pulmonary vein at the posterior wall of the left atrium (horn‑like insertion) is absent, which leads to a completely smooth posterior wall in the four-chamber view [6,7]. The “twig sign” represents the entry of the pulmonary veins into a confluent chamber behind the left atrium [7], and is visible in the four‑chamber view except in the cardiac type. In the cardiac type, the confluent vein is located more inferiorly, below the plane of the four‑chamber view and does not form a twig sign, making it more difficult to detect [5]. In supracardiac TAPVR, an ascending vertical vein can be observed in the 3-vessel tracheal view as an additional vessel, usually located at the left of the main pulmonary artery. In infracardiac TAPVR, the descending vertical vein can be seen as an additional vein in the axial abdominal plane [8].
In many cases, direct signs are not visualized, thus identification of indirect signs allow us to suspect this pathology, not diagnose it. They are based on morphological findings such as increased post‑left atrium space, or on hemodynamic changes such as ventricular disproportion, dilated superior vena cava or coronary sinus, and abnormal Doppler waveforms. The presence of a pulmonary venous confluence leads to an increased distance between the left atrium (LA) and the descending aorta (DAo) [9]. While visualization of the confluent chamber may be difficult, objectively measuring the increase in the space behind the left atrium in an axial section may be easier to verify. Various indices have been proposed for this purpose, the most widely used being the “post‑LA space index” described by Kawazu et al [10]. It is calculated as the ratio of the LA‑DAo distance to the diameter of the DAo, proposing a value ≥1.27 as a potential marker of TAPVR. In clinical practice, a cut-off of 1.0 may be more useful to increase detection rates, although this would be at the expense of more false positives. An alternative marker with a similar diagnostic performance and independent of the gestational age is the “left atrial posterior space to diagonal ratio,” which is calculated by dividing the LA‑DAo distance by the left atrial diameter, with an optimal cut-off ≥0.35 [11]. Asymmetric ventricular chamber dimensions with right heart dominance result from extra‑abnormal flow from the pulmonary veins to the right heart, providing a diagnostic clue for TAPVR [9], but this finding is late and not very specific. In supracardiac TAPVR, anomalous pulmonary venous drainage increases blood flow to the collector, which travels to the right atrium through the dilated innominate vein and superior vena cava, visible in the three-vessel trachea and bicaval views [7,12]. In the subcostal view of pediatric echocardiography, the cardiac type is characterized by the “whale’s tail sign,” where left and right pulmonary veins drain into the dilated coronary sinus. Although it is a technically difficult plane to obtain in fetal echocardiography, it has been described by Karmegaraj in a 25-week-old fetus [13]. Spectral Doppler waveforms are typically normal or biphasic in cardiac type, whereas in supracardiac and infracardiac types, the waveforms can be biphasic, monophasic, or continuous [6,7]. Color and spectral Doppler assessment allows the identification of the fetuses with pulmonary venous pathway obstruction and, therefore, at risk for acute postnatal deterioration with severe respiratory distress and cyanosis [14].
During intrauterine life, the malformation does not compromise the fetal circulation, since the patent foramen ovale provides easy access of right atrial blood to the left side of the heart and pulmonary blood flow is a small portion of the combined ventricular output. In fetuses with severe pulmonary venous obstruction, their condition is critical at birth and requires immediate cardiology and cardiac surgery attention since after the foramen ovale closes, oxygenated blood does not return to the left atrium, left ventricle, and aorta. Early prenatal detection of this heart defect enables an optimal plan for monitoring and treatment of the condition, and significantly influences the prognosis [14,15].
References
[1] Abuhamad A, Chaoui R. Anomalies of Pulmonary Venous Connections. In: A practical guide to fetal echocardiography: normal and abnormal hearts, 4th ed. Wolters Kluver, Philadelphia, PA, 2022; pag 680-699.
[2] Correa-Villaseñor A, Ferencz C, Boughman JA, Neill CA. Total anomalous pulmonary venous return: familial and environmental factors. The Baltimore-Washington Infant Study Group. Teratology. 1991 Oct;44(4):415-28.
[3] Craig JM, Darling RC, Rothney WB. Total pulmonary venous drainage into the right side of the heart; report of 17 autopsied cases not associated with other major cardiovascular anomalies. Lab Invest. 1957 Jan-Feb;6(1):44-64.
[4] Bakker MK, Bergman JEH, Krikov S, et al. Prenatal diagnosis and prevalence of critical congenital heart defects: an international retrospective cohort study. BMJ Open. 2019 Jul 2;9(7):e028139.
[5] Chih WL, Ko H, Chang TY. Prenatal Ultrasound Markers of Isolated Total Anomalous Pulmonary Venous Return and a Sequential Approach to Reach Diagnosis. J Med Ultrasound. 2024 Apr 26;32(2):104-109.
[6] Tongsong T, Luewan S, Jatavan P, et al. A Simple Rule for Prenatal Diagnosis of Total Anomalous Pulmonary Venous Return. J Ultrasound Med. 2016 Jul;35(7):1601-7.
[7] Ganesan S, Brook MM, Silverman NH, Moon-Grady AJ. Prenatal findings in total anomalous pulmonary venous return: a diagnostic road map starts with obstetric screening views. J Ultrasound Med. 2014 Jul;33(7):1193-207.
[8] Patel CR, Lane JR, Spector ML, et al. Totally anomalous pulmonary venous connection and complex congenital heart disease: prenatal echocardiographic diagnosis and prognosis. J Ultrasound Med. 2005 Sep;24(9):1191-8.
[9] Paladini D, Pistorio A, Wu LH, et al. Prenatal diagnosis of total and partial anomalous pulmonary venous connection: multicenter cohort study and meta-analysis. Ultrasound Obstet Gynecol. 2018 Jul;52(1):24-34.
[10] Kawazu Y, Inamura N, Kayatani F, Taniguchi T. Evaluation of the post-LA space index in the normal fetus. Prenat Diagn. 2019 Feb;39(3):195-199.
[11] Anuwutnavin S, Unalome V, Rekhawasin T, et al. Fetal left-atrial posterior-space-to-diagonal ratio at 17-37 weeks' gestation for prediction of total anomalous pulmonary venous connection. Ultrasound Obstet Gynecol. 2023 Apr;61(4):488-496.
[12] Volpe P, Campobasso G, De Robertis V, et al. Two- and four-dimensional echocardiography with B-flow imaging and spatiotemporal image correlation in prenatal diagnosis of isolated total anomalous pulmonary venous connection. Ultrasound Obstet Gynecol. 2007 Nov;30(6):830-7.
[13] Karmegaraj B. Whale's tail sign in fetus with coronary sinus total anomalous pulmonary venous connection. Ultrasound Obstet Gynecol. 2023 Nov;62(5):761-764.
[14] Valsangiacomo ER, Hornberger LK, Barrea C, et al. Partial and total anomalous pulmonary venous connection in the fetus: two-dimensional and Doppler echocardiographic findings. Ultrasound Obstet Gynecol. 2003 Sep;22(3):257-63.
[15] Domadia S, Kumar SR, Votava-Smith JK, Pruetz JD. Neonatal Outcomes in Total Anomalous Pulmonary Venous Return: The Role of Prenatal Diagnosis and Pulmonary Venous Obstruction. Pediatr Cardiol. 2018 Oct;39(7):1346-1354.
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Javier Cortejoso Spain Physician

Padman KG United Kingdom Sonographer

Pawel Swietlicki Poland Physician

Chursina Olga Russian Federation Physician

belen garrido Spain Physician

Alexandr Krasnov Ukraine Physician

Andres Arencibia United States Physician

Mayank Chowdhury India Physician

Vladimir Lemaire United States Physician

Boujemaa Oueslati Tunisia Physician

Tatiana Koipish Belarus Physician

carlos lopez Venezuela Physician

CHARLES SARGOUNAME India Physician

Aysegul Ozel Turkey Physician

Rushina Patel United States Sonographer

Caroline Reichert Garcia Brazil Physician

PRIYA R United States Physician

Laura Currie United States

Kimberly Delaney United States Sonographer

Olivia Ionescu United Kingdom Physician

Marianovella Narcisi Italy Physician

Javier Ayala Spain Physician

SUNIL SHAH India Physician

Rebecca Evans Australia Sonographer
Giap Hoang Anh Viet Nam Physician

CHEN YANG China Physician

Amparo Gimeno Spain Physician

Elena Andreeva Russian Federation Physician

Muradiye YILDIRIM Turkey Physician

Ta Son Vo Viet Nam Physician

ALBANA CEREKJA Italy Physician

Eti Zetounie Israel Sonographer

Deval Shah India Physician

Murat Cagan Turkey Physician

ANA PAULA PASSOS Brazil Physician

GOYAL MANISH United States

Büşra Cambaztepe Turkey Physician

Ionut Valcea Romania Physician

Sviatlana Akhramovich Belarus Physician

Đặng Mai Quỳnh Viet Nam Physician

Halil Korkut Dağlar United States Physician

Hien Nguyen Van Viet Nam Physician

Kathrine Montagne United States Sonographer

Almaz Kinzyabulatov Russian Federation Physician

Zuzana Briešková Slovakia Physician

Dr Monika Sharma India Physician

András Weidner Hungary Physician

Ann-Christin Dr. Sönnichsen Germany Physician

Maria Kuznetsova Russian Federation Physician

Annette Reuss Germany Physician
shruti Agarwal India Physician

Vu The Anh Viet Nam Physician
Jay Vaishnav India Physician

YULIA VISHNEVSKAYA Russian Federation Physician

Nguyen Xuan Cong Viet Nam Physician

Navya KC India Physician

Poojitha Alladi India Physician

shay kevorkian Israel Physician

Manjula Budidapadu India Physician
Qi Tang China Physician

Harshal Patil India Physician

Sruthi Pydi India Physician

zozo sichala Zambia radiology technologist

Sara Settepani United States Sonographer

Rupal Sasani India Physician

Joanna Głowska-Ciemny Poland Physician

Petra Barboríková Slovakia Physician

Denys Saitarly Israel Physician

Le Tien Dung Viet Nam Physician

Tetiana Ishchenko Ukraine Physician

Costin Radu Lucian Romania Physician

Le Duc Viet Nam Physician

Janaina Andrade Brazil Physician

Philippe Viossat Antarctica Consultant

Hana Habanova Slovakia Physician

Purvi Agrawal India Physician

Jagdish Suthar India Physician

Katsiaryna Adamenko France Physician

Lauren Carlos United States Physician

ASHLEA HARDIN United States Sonographer

sugunadevi Viswanathan India Physician

Ali Ozgur Ersoy Turkey Physician

Gökçen Örgül Turkey Physician

Lucia Bobik Slovakia Physician

ZHANNA Kurmangaliyeva Kazakhstan Physician

Surekha Bhimangouda India Physician

Homam Saker United States Physician

yongling jiang China Physician

Charmi Prajapati India Sonographer

Sergey Shumakov Russian Federation Physician

KIM SOCHETRA Cambodia Physician

Henrietta Karlsson Spain Physician

Young-Mi Lee United States Physician

Jeanine Coetzer Australia Sonographer

Jaimee Blood United States Sonographer

Nadya klinin Israel Sonographer

Ngoc Bich Viet Nam Physician

Monika Pasieczna Poland Physician

Dang Thinh Nguyen Viet Nam Physician