Case of the Week #582
(1) Femicare, Center of prenatal ultrasonographic diagnostics, Matrtin, Slovakia; (2) Centro Médico Recoletas, Valladolid, Spain


View the Answer Hide the Answer
Answer
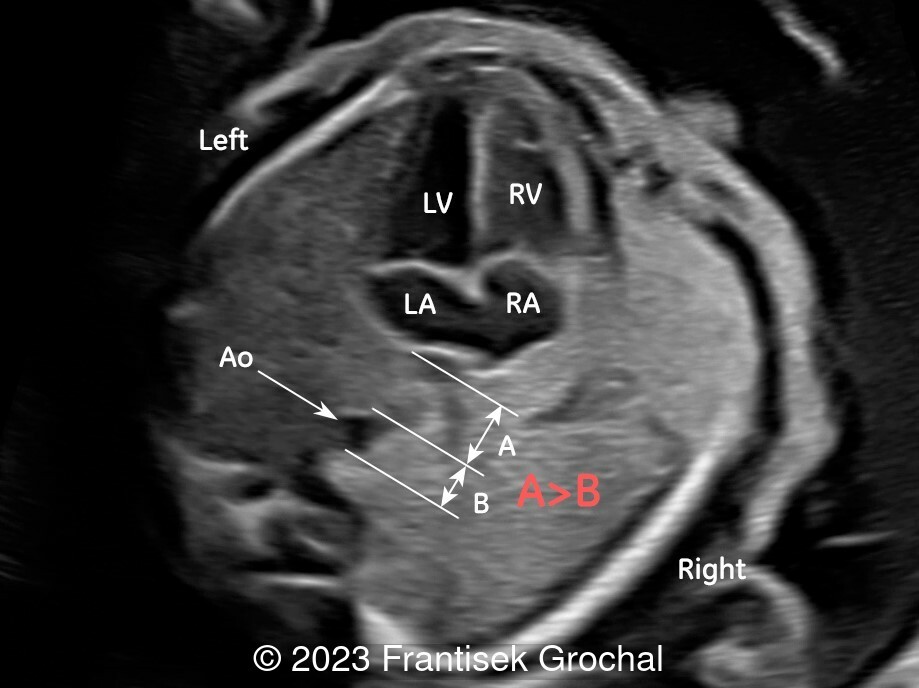
We present a case of Total Anomalous Pulmonary Venous Connection (TAPVC), supra-cardiac type. The pulmonary veins led to a confluent vein behind the left atrium, and the venous flow continued via an ascendant vertical vein to the superior vena cava. No other anomalies were found. The patient was referred to our national cardiac center, where delivery and management of the baby is planned.
Left atrial space cut-off value of 1.0 is recommended for prenatal diagnosis of TAPVC, with sensitivity of 100% and specificity of 89% [1].

Discussion
The fundamental characteristic of congenital anomalies of the pulmonary venous connections is failure of the pulmonary veins to establish a normal connection to the left atrium. Instead, they either drain directly or through the systemic veins to the right atrium [2,3]. Although the terms "connection," "drainage" or "return" are used interchangeably, the first more accurately describes the anatomical characteristics of the anomaly [4]. Total anomalous pulmonary venous connection (TAPVC) is characterized by the anomalous drainage of all four pulmonary veins, whereas partial anomalous pulmonary venous connection (PAPVC) is characterized by the anomalous drainage of one, two, or three of the pulmonary veins. Of all the variants of partial anomalous pulmonary venous connection, the one most frequently diagnosed is associated with scimitar syndrome, which is characterized by hypoplasia of the right lung, hypoplasia of the right pulmonary artery, dextroposition, and anomalous drainage of right inferior pulmonary vein to the inferior vena cava [5].
The failure of the primitive pulmonary vein to connect to the primitive pulmonary venous splanchnic plexus, and the subsequent incorporation of the pulmonary venous sinus to the roof of the left atrium gives rise to an anomalous pulmonary venous connection [6]. The incidence of total anomalous pulmonary venous connection in the general population is approximately 1 in 10,000 live births, and 2% of all congenital heart disease [7]. It may be isolated, but is commonly associated with heterotaxy syndromes, specifically right isomerism. Rarely, it has been associated with cat-eye syndrome, Holt–Oram syndrome, and Noonan syndrome [3].
The first review of the anatomic characteristics of total anomalous pulmonary venous connection was published by Brody in 1942 [8]. Craig et al. [9] categorized this pathology into four types depending on the site of the connection to the systemic veins. These are, in decreasing order of frequency [10]:
- Type 1, supracardiac (50%): the four pulmonary veins drain into a venous collector located behind the left atrium, from which a vertical vein travels up to reach the innominate vein, the superior vena cava or, more rarely, the azygos vein.
- Type 2, cardiac (25%): the pulmonary veins drain through the coronary sinus or directly into the right atrium.
- Type 3, infracardiac (16%): the pulmonary veins drain into a confluence that connects to a vertical vein, which runs down the side of the esophagus, passes through the diaphragm, and drains into the portal vein.
- Type 4, mixed (9%): a large variety of pulmonary venous drainage patterns may occur in this subgroup.
In the normal fetus, at least the two inferior pulmonary veins can be identified entering the left atrium on an apical or a subcostal four-chamber views. The two superior pulmonary veins are usually more difficult to appreciate. The use of color Doppler can be helpful. It is necessary to decrease the velocity scale or pulse repetition frequency (PRF) to 10-20 cm/sec to clearly identify the entry of the veins into the left atrium [11]. The diagnosis of total anomalous pulmonary venous connection can be excluded if one or more of the four pulmonary veins terminate normally in the left atrium. Unless all four normal connections are identified entering the left atrium, the diagnosis of partial anomalous pulmonary venous connection cannot be excluded [12].
Prenatal diagnosis of total anomalous pulmonary venous connection is particularly difficult when it is isolated, with only 2% to 10% of all cases being diagnosed before birth, usually in the third trimester of pregnancy [13,14]. Indirect and direct echocardiographic signs suggesting its prenatal diagnosis have been well described in numerous publications [4, 14-16]. Indirect signs of total anomalous pulmonary venous connection are moderate ventricular disproportion, with the right chambers larger than the left ones (not visible until the third trimester), and an enlarged pulmonary artery compared to the ascending aorta. The fetal echocardiographic clues to the diagnosis of total anomalous pulmonary venous connection include:
- Failure to demonstrate a direct pulmonary venous connection to the left atrium (and, therefore, a smooth posterior wall of the atria)
- The detection of a venous confluence chamber behind the left atrium (called “confluent vein”, “twig sign”, or “starfish sign” by different authors [3,17,18])
- Increased distance between the left atrium and the descending aorta [14].
Kawazu et al [1] evaluated the ratio of the left atrium–descending aorta distance to the diameter of the descending aorta (‘post-LA space index’) in 101 normal and eight total anomalous pulmonary venous connection fetuses, finding a significantly higher value (>1.27) in pathological cases. In addition to the signs common to all types of total anomalous pulmonary venous connection, there are other signs specific to the type. In the the supracardiac type, these include an ascending vertical vein as a fourth vessel in the three-vessel-trachea view and dilated left brachycephalic/superior cava veins. In the cardiac type, a dilated coronary sinus can be visualized, and in the infracardiac type, a vertical vein descending into the liver from the lung can be demonstrated [3].
Color and spectral Doppler are essential for the evaluation of the normal and abnormal connections of the pulmonary veins. Obstruction to pulmonary venous return can occur at any level between the pulmonary veins and the right atrium. It is nearly universal in the infradiaphragmatic type. In the supracardiac type, drainage is obstructed in approximately 40% of patients, and in the cardiac type total anomalous pulmonary venous connection is only occasionally obstructed [2]. When color Doppler imaging reveals turbulence in the vertical vein, or at connection sites, the possibility of an obstructed total anomalous pulmonary venous connection should be considered. Spectral Doppler interrogation of the pulmonary veins shows different waveforms than those found in the pulmonary veins normally connected to the left atrium and can be characterized by a either abnormal appearance, biphasic with decreased pulsatility, monophasic but pulsatile, and monophasic and nonpulsatile [17].
Fetal shunts allow total anomalous pulmonary venous connection to be well tolerated in utero. After birth, there is complete mixing of the pulmonary and systemic circulations in the right heart, and the infant will be cyanotic. In some neonates, the presence of an obstructive abnormal pulmonary venous return can cause respiratory distress and decompensation very early in the neonatal period [2]. Despite this, the overall prognosis is good for neonates who survive surgical correction.
Differential diagnosis [4,16,19] includes other causes of right-to-left heart size discrepancy, such as aortic coarctation. In the supracardiac total anomalous pulmonary venous connection, the vertical vein can be confused with a persistence of the left superior vena cava. Color Doppler demonstrating a cranial to caudal direction of flow in the persistent left superior vena cava is helpful. Inferior vena cava interruption with azygos continuation results in dilated azygos vein posterior to the left atrium, which may be confused for a confluent vein. The key to diagnosis is demonstrating the lack of continuity between the left atrium and the pulmonary veins, which is not always easy.
References
[1] Kawazu Y, Inamura N, Shiono N, et al. 'Post-LA space index' as a potential novel marker for the prenatal diagnosis of isolated total anomalous pulmonary venous connection. Ultrasound Obstet Gynecol. 2014 Dec;44(6):682-7. doi: 10.1002/uog.13357.
[2] Moon-Grady AJ. Pulmonary vein anomalies. In: Yagel S, Silverman N, and Gembruch U, ed. Fetal Cardiology. Embryology, Genetics, Physiology, Echocardiographic Evaluation, Diagnosis and Perinatal Management of Cardiac Diseases, 3rd ed. CRC Press, Taylor & Francis Group, Boca Raton, FL, 2019; pages 263-274.
[3] Abuhamad A, Chaoui R. Anomalies of Pulmonary Venous Connections. In Abuhamad A and Chaoui R, ed. A practical guide to fetal echocardiography: normal and abnormal hearts, 4th ed. Wolters Kluver, Philadelphia, PA, 2022; pages 680-699.
[4] Escribano D, Herraiz I, Galindo A. Anomalías congénitas del drenaje venoso pulmonar. In: Galindo A, Gratacós E and Martínez JM. Cardiología fetal. Marbán, Madrid, 2015; pages 272-288.
[5] Grisaru D, Achiron R, Lipitz S, et al. Antenatal sonographic findings associated with scimitar syndrome. Ultrasound Obstet Gynecol. 1996 Aug;8(2):131-3. doi: 10.1046/j.1469-0705.1996.08020131.x.
[6] Muñoz Castellanos L, Kuri Nivón M, Sánchez Vargas CA, et al. Conexión anómala de venas pulmonares. Correlación anatomoembriológica [Anomalous pulmonary venous connection]. Arch Cardiol Mex. 2008 Jul-Sep;78(3):247-54.
[7] Grabitz RG, Joffres MR, Collins-Nakai RL. Congenital heart disease: incidence in the first year of life. The Alberta Heritage Pediatric Cardiology Program. Am J Epidemiol. 1988 Aug;128(2):381-8. doi: 10.1093/oxfordjournals.aje.a114978.
[8] Brody H. Drainage of the pulmonary veins into the right side of the heart. Arch Path. 1942; 33:221-240.
[9] Craig JM, Darling RC, Rothney WB. Total pulmonary venous drainage into the right side of the heart; report of 17 autopsied cases not associated with other major cardiovascular anomalies. Lab Invest. 1957 Jan-Feb;6(1):44-64.
[10] Seale AN, Uemura H, Webber SA, et al; British Congenital Cardiac Association. Total anomalous pulmonary venous connection: morphology and outcome from an international population-based study. Circulation. 2010 Dec 21;122(25):2718-26. doi: 10.1161/CIRCULATIONAHA.110.940825.
[11] Chaoui R, Lenz F, Heling KS. Doppler examination of the fetal pulmonary venous circulation. In: Maulick D, ed. Doppler Ultrasound in Obstetrics and Gynecology. Springer Verlag, Berlin, 2003; pages 451-463.
[12] Stamm ER. Anomalous Pulmonary Venous Connection. In: Drose JA, ed. Fetal echocardiography, 2nd ed. Saunders Elsevier, St. Louis, MO, 2010; pages 245-255.
[13] Seale AN, Carvalho JS, Gardiner HM, et al; British Congenital Cardiac Association. Total anomalous pulmonary venous connection: impact of prenatal diagnosis. Ultrasound Obstet Gynecol. 2012 Sep;40(3):310-8. doi: 10.1002/uog.11093.
[14] Laux D, Fermont L, Bajolle F, et al. Prenatal diagnosis of isolated total anomalous pulmonary venous connection: a series of 10 cases. Ultrasound Obstet Gynecol. 2013 Mar;41(3):291-7. doi: 10.1002/uog.11186.
[15] Allan LD, Sharland GK. The echocardiographic diagnosis of totally anomalous pulmonary venous connection in the fetus. Heart. 2001 Apr;85(4):433-7. doi: 10.1136/heart.85.4.433.
[16] Volpe P, Campobasso G, De Robertis V, et al. Two- and four-dimensional echocardiography with B-flow imaging and spatiotemporal image correlation in prenatal diagnosis of isolated total anomalous pulmonary venous connection. Ultrasound Obstet Gynecol. 2007 Nov;30(6):830-7. doi: 10.1002/uog.5145.
[17] Ganesan S, Brook MM, Silverman NH, et al. Prenatal findings in total anomalous pulmonary venous return: a diagnostic road map starts with obstetric screening views. J Ultrasound Med. 2014 Jul;33(7):1193-207. doi: 10.7863/ultra.33.7.1193.
[18] Lee W, Espinoza J, Cutler N, et al. The 'starfish' sign: a novel sonographic finding with B-flow imaging and spatiotemporal image correlation in a fetus with total anomalous pulmonary venous return. Ultrasound Obstet Gynecol. 2010 Jan;35(1):124-5. doi: 10.1002/uog.7503.
[19] Bravo-Valenzuela NJM, Peixoto AB, Araujo Júnior E. Prenatal diagnosis of total anomalous pulmonary venous connection: 2D and 3D echocardiographic findings. J Clin Ultrasound. 2021 Mar;49(3):240-247. doi: 10.1002/jcu.22973.
Discussion Board
Winners
Dr. Hitanshu Bhatt India Physician

ahmed gohar United States Physician

Javier Cortejoso Spain Physician

Luis Izquierdo United States Physician

Umber Agarwal United Kingdom Maternal Fetal Medicine
Anna Meshkova Russian Federation Physician
Igor Yarchuk United States Sonographer

Larysa Gazarova United States Physician

belen garrido Spain Physician
Dr.Neel Vaghasia India Physician

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Alexandr Krasnov Ukraine Physician

Mayank Chowdhury India Physician

Michaela Apostolou Germany Physician

filiz halici öztürk Turkey Physician

Oskar Sylwestrzak Poland Physician

Vladimir Lemaire United States Physician
Ivan Ivanov Russian Federation Physician

Boujemaa Oueslati Tunisia Physician

Tatiana Koipish Belarus Physician

carlos lopez Venezuela Physician
CHARLES SARGOUNAME India Physician

Aysegul Ozel Turkey Physician
Halil Mesut Turkey Physician
Anita Silber Israel Physician
Kimberly Delaney United States Sonographer

Olivia Ionescu United Kingdom Physician

Javier Ayala Spain Physician
Luis Cadena Venezuela Physician

Crismaru Iulia Romania Physician

Annette Reuss Germany Physician

Muradiye YILDIRIM Turkey Physician

ALBANA CEREKJA Italy Physician
Selvanandhini Gopalasundaram India Physician

Murat Cagan Turkey Physician

Loai Said Palestinian Territory, Occupied Physician

gholamreza azizi Iran, Islamic Republic of Physician

Ionut Valcea Romania Physician
KHALED RAMADAN Egypt Physician

Malgorzata Kowalska Poland Physician

Kathrine Montagne United States Sonographer

Tito Gruhn United States Physician

Daniil Gagaev Russian Federation Physician

Yao Shifa China Physician

Mariam Bamanie Saudi Arabia Physician

Vandana Yakub India Physician
shruti Agarwal India Physician

Perrine Riou-Kerangal French Polynesia Sage-femme échographiste

Deniz OLUKLU Turkey Physician

Mai Phương Viet Nam Physician

Yogesh Chinnawar India Physician
mohamed ateya Egypt Physician

Kedarnath Dixit India Physician
Qi Tang China Physician

Lynn Davis United States Sonographer

lei zhou China Sonographer

Andrea Stoop-Berends Netherlands Sonographer

Ismail Guzelmansur Turkey Physician

Alesia Haidalenok Belarus Physician

Tuuli Haabpiht Estonia Physician

Harshal Patil India Physician

LiJen FAN Taiwan, Province of China Sonographer

Mina Dawod United States Medical Student

jayeta choudhury India Physician

TUYEN LE KIM Viet Nam Physician

Sruthi Pydi India Physician

Chantel Morrell United States Sonographer

Manoj Pokhrel Nepal Physician

Zachary Brown United States Sonographer